PARATORMONE (PTH)
Parathormone is produced when the blood calcium level is low; it is secreted by the parathyroid cells, which are in contact with the thyroid tissue. It is a small protein of 84 amino acids synthesized as preproPTH and accumulated in granules, so-called secretion vesicles.

In parathyroid cells if plasma calcium is high this results, (via a seven-step, G-protein bound calcium sensor receptor) in the activation of phospholipase C and the formation of inositol 3P which results in the release of calcium from the endoplasmic reticulum and an increase in intracellular calcium. Intracellular calcium inhibits, in this case, the release of parathormone from secretory vesicles; this is one of the few cases in which calcium inhibits anything. If, on the other hand, extracellular calcium is low, it increases parathormone synthesis and secretion, via the PKA and cAMP pathway. Vitamin D, or calcitriol, inhibits parathormone release, this is because PTH stimulates vitamin D production. Being a protein, parathormone has a very low stay in the circulation, acting on bone, kidney and indirectly on the intestine. The kidney is the central organ in calcium regulation, PTH determines the fine tuning of this renal function. Sixty-five percent of filtered calcium is reabsorbed in the proximal tubule in a constitutive, unregulated manner, together with sodium and H2O; approximately 20% of filtered calcium is reabsorbed in the ascending tract of Henle's loop, and approximately 15% of filtered calcium is reabsorbed in the distal convoluted tubule, under control of PTH. The excreted portion is quantitatively minimal, approximately 0.2 g/day out of 10 g/day of ultrafiltrate, i.e., 2%. Therefore, at the level of the kidney, parathormone stimulates an increased reabsorption of calcium in the distal tubule, but there is also, above all, an increased release of phosphate in the proximal tubule.
The entry of calcium is due to the transport of calcium channels on the membrane; calcium cannot leave the cell on the luminal side because on the basal side are synthesized and exposed transporters that clearly transport calcium in the blood, instead the parathormone in the proximal tubule binds to the receptor, activates PKA and allows the withdrawal of phosphate transporters from the membrane (they are sodium-phosphate cotransporters) thus preventing phosphate from being reabsorbed. In addition, KREB is activated, which stimulates the synthesis of 1-alpha-hydroxylase, which catalyzes vitamin D synthesis. Finally on bone, osteoclasts are not directly stimulated, as they do not have a receptor, but instead osteoblasts are stimulated, which increase the levels of MCSF, RANK-L and lower the levels of OSTEOPROTEGERIN, which serves to increase the number of osteoclasts that will digest more bone. Thus, PTH stimulates the resorption of bone by osteoclasts and the subsequent release of calcium and phosphate into the interstitial fluid. The level of calcium and phosphate thus increases but there is no precipitation because in the kidney calcium is absorbed at the proximal convoluted tubule in a constitutive manner and phosphate is excreted.
Finally, PTH stimulates the synthesis of prostglandins in osteoblasts that have a function in bone resorption. With regard to the intestine, parathormone also increases renal 1-alpha-hydroxylase activity, with increased production of 1,25-hydroxy-vitamin D and increased absorption of calcium and inorganic phosphate by the small intestine. Thus, PTH also activates vitamin D, which in turn stimulates calcium absorption.
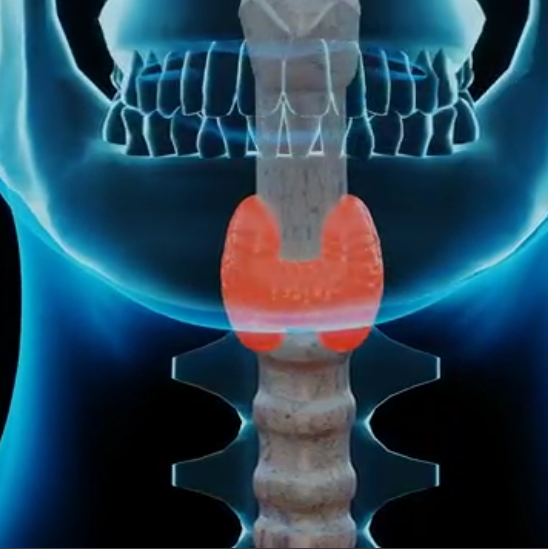
![]() Paratormone PTH
Paratormone PTH