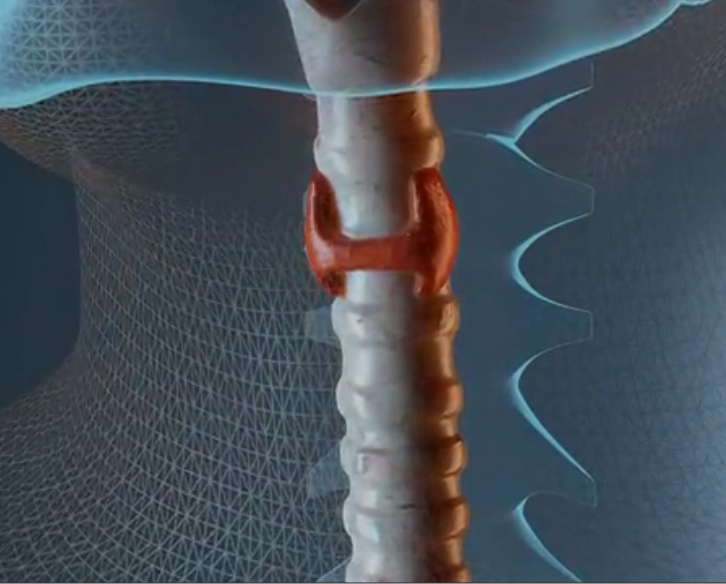
The thyroid
The thyroid is an endocrine organ consisting of follicular cells surrounding a glandular area in which thyroglobulin accumulates.
The thyroid is part of the physiological system that connects the central nervous system with the peripheral organs. This takes place at the level of an axis called "hypothalamic-pituitary axis" that allows to regulate, through a series of hormones, peripheral activities.
The cerebral cortex receives stimuli from outside and, depending on conditions, processes signals for our body to respond. The hypothalamus is a part of the nervous system that is very important in communicating and processing sensory signals from outside. It is able to release a series of polypeptides that are generally called "realasing hormons" that act on the cells of the adenohypophysis and induce, depending on their specificity, the release of hormones. In the specific case of the thyroid, the hypothalamus produces TRH (thyrotropic realising hormon) which is a small polypeptide of three amino acids that activates the thyrotropic cells of the adenohypophysis to produce TSH (thyroid stimulating hormon). The latter induces at thyroid level the production of the two thyroid hormones T3 and T4 that act on peripheral targets.

Thyroid hormones are derived from the amino acid tyrosine. In the image to the left, tyrosine and the composition of thyroid hormones can be seen. Tyrosine is present but the alcohol group of the phenolic ring is linked to another phenolic ring. These two rings in the T3 and T4 hormone are bound to 3 and 4 iodine molecules, respectively. Looking closely at the arrangement, we can deduce the numbering that from the number 3 and 5 corresponds to the phenolic ring bound to the alpha carbon of the amino acid, while the numbering 3' and 5', indicates the iodinated carbon in the secondary phenolic ring. So T4 has 4 iodinated residues while T3 has 3 where two are present on the "real" tyrosine ring and one on the accessory ring.
The precursors of thyroid hormones are tyrosines that are in a protein secreted by follicular cells stimulated by TSH. This protein is thyroglobulin and is a highly glycosylated glycoprotein, consisting of two chains with very high molecular weight (660000 daltons). Its iodine content is proportional to the concentration of iodine present in the plasma and, therefore, proportional to the amount of iodine we introduce with the diet.
Only 40 tyrosine residues are able to bind iodine. To define which tyrosine is iodinable it is necessary that it is surrounded by a consensus sequence, that is there must be flanked by a series of selective and specific amino acids. A tyrosine without such flanking features will be difficult to iodinate.
The thyroid produces T3 and T4 but the concentrations are not equimolar. Basically T4 is produced 16 times more. The reason of this situation is explained because T3, from the biological point of view, is much more active than T4 and, moreover, T3 is the real hormone able to induce the genetic program predisposed by this type of stimulus. T4 is a form of pre-hormone at ready availability directly present in the circulation and therefore at more rapid use.
Once secreted by the thyroid gland, thyroid hormones, circulate in the bloodstream bound to transporter proteins. These are thyroid hormone-binding globulin, which binds about 70% of the hormones, and then transiterin and albumin bind 15%, respectively. Thyroid hormones only act when they are not bound to these proteins, either T3 as a truly effector hormone or T4 as a circulating precursor. In other words, T4 cannot be de-iodinated when bound to these types of proteins.
Thyroid hormones act like steroid hormones, vitamin D and ethinoic acid, that is, they go to modulate transcription. The endocellular receptors that bind the above mentioned molecules are able to regulate the transcription process. These nuclear receptors always have a domain capable of specifically recognizing its ligand (ethinoic acid, steroid hormones, etc. ...). They also have a portion that binds the DNA and one that goes to regulate the function of the receptor when it must bind the ligand or another monomer to form a heterodimer. T3 and T4 enter and are metabolized or catabolized. T3 is the true effector and the heterodimer RXR (receptor for thyroid hormone) has a repressor value on transcription, in fact it binds a corepressor that goes to occupy the sites of the promoter of those genes that are sensitive to this heterodimer. The arrival of T3 induces a change of shape of the heterodimer causing loss of affinity for the co-repressor. In this way the transcription can start because, instead of binding the co-repressor, it binds the various activators of transcription. So a transcriptional signal starts that induces a change in the cell's gene surround. The end result is to increase basal metabolism and basically stimulate growth and survival of various tissues.
In addition, some metabolic actions occur: for example, glucose reabsorption, increased oxidative phosphorylation, transcription of a number of enzymes, adrenal activity with the production of catacolamines and utilization (take) of glucose. There is also a more general action on the mechanisms of the hypothalamic-pituitary axis based on growth, in fact, it is required for the action of growth hormone and prolactin.
Thyroid hormone activity is ubiquitous but, nevertheless, there are systems that are more stimulated, i.e., their effect is more pronounced. At the level of the cardiovascular system, thyroid hormones have a profound effect on cardiac function both as a positive inotropic effect and as a positive chronotropic effect. In the CNS a deficiency of thyroid hormones during development and the first years of life induces a mental retardation while in the hyperthyroid patient it is a habitus of hyperactivity, hyperexcitability and anxiety. The effect on the reproductive system (on prolactin, mentioned above) is wide-ranging and hypothyroid patients who are not adequately treated have problems of reduced or absent fertility.
They also have an impact on protein turnover both as a negative and a positive regulator: under conditions of low concentrations of thyroid hormone, protein synthesis increases while, in the opposite situation, protein catabolism is promoted. Regarding sugar metabolism, low doses cause an increase in glycogen synthesis and high doses increase glycogen catabolism. For lipids, mobilization of fatty acids from adipose tissue increases, as well as beta-oxidation, and an inverse correlation between circulating cholesterol levels and thyroid hormone levels is always observed (this is a clinical fact for endocrinologists): low thyroid hormone = high cholesterol and vice versa.
![]() Tiroide
Tiroide