| "Descrizione" by Al222 (24136 pt) | 2025-Apr-01 12:08 |
Lactulose is a synthetic disaccharide composed of two monosaccharides: galactose and fructose. It is produced through the chemical transformation of lactose, a natural sugar found in milk. Lactulose is primarily used as a laxative and for the treatment of intestinal disorders, but it is also applied in other pharmaceutical and food-related fields.
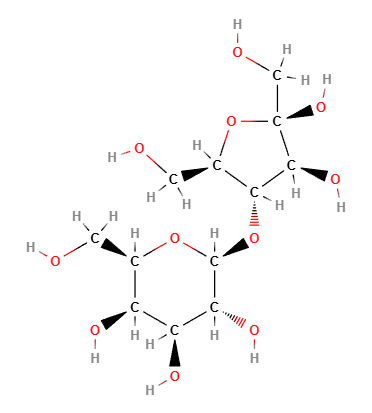
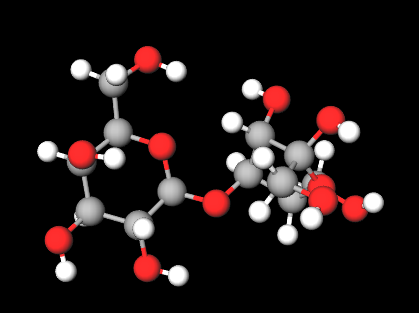
Chemical Composition and Structure
Lactulose is a disaccharide consisting of two monosaccharides:
Galactose: A monosaccharide derived from lactose.
Fructose: A monosaccharide naturally found in many fruits.
Its chemical formula is C₆H₁₂O₆, and its structure is composed of two sugars linked by a glycosidic bond that the human digestive system cannot break down.
Physical Properties
Appearance: Lactulose appears as a white, crystalline powder or syrup.
Solubility: It is highly soluble in water, making it easy to use in aqueous solutions.
Odor: Lactulose has a very mild or no odor.
Taste: It has a sweet taste, though it is less sweet than sucrose (table sugar).
Benefits and Functions
Laxative: Lactulose is widely used as an osmotic laxative. It is not absorbed in the small intestine and passes into the colon, where it is fermented by bacteria, producing acids that increase water content and promote bowel movements, easing constipation (1).
Treatment of constipation: It is used to treat chronic constipation and in situations where gentle stimulation of the intestines is needed.
Treatment of hepatic encephalopathy: Lactulose is used to reduce ammonia levels in the blood of patients with hepatic encephalopathy. It works by reducing ammonia production in the colon, which would otherwise accumulate in the body (2).
Prebiotic: Lactulose acts as a prebiotic, promoting the growth of beneficial gut bacteria and improving overall gut health.
Regulating intestinal pH: The use of lactulose can lower intestinal pH, creating an environment favorable for the growth of beneficial bacteria and inhibiting the growth of pathogenic bacteria.
Applications
Pharmaceutical Industry
Laxative: Lactulose is primarily used in medications to treat constipation. It is available in syrup, tablet, or powder form to be dissolved in water.
Treatment for hepatic encephalopathy: It is used in patients with severe liver disease to treat hepatic encephalopathy by reducing ammonia in the blood.
Gut health supplements: Lactulose is used as a prebiotic in some dietary supplements to improve gut health.
Food Industry
Sweetener: Lactulose is sometimes used as a sweetener in food products, particularly in diabetic-friendly products, as it has a minimal impact on blood sugar levels.
Gut health products: It is used in functional foods intended to promote gut health, such as yogurt and dietary supplements.
Cosmetics and Personal Care
Moisturizing agent: Because lactulose is water-soluble, it is used in some cosmetic formulations as a humectant, helping to hydrate the skin.
Prebiotic for the skin: Some skincare products contain lactulose as a prebiotic to stimulate the growth of beneficial bacteria on the skin.
Environmental and Safety Considerations
Biodegradability: Lactulose is fully biodegradable, making it an eco-friendly option for various uses.
Safety: Lactulose is generally considered safe for use as a laxative and prebiotic supplement. However, excessive use can lead to side effects such as flatulence, abdominal cramps, or diarrhea. It should be used with caution in people with certain intestinal conditions.
Sustainability: Since lactulose is derived from lactose, a natural resource, its production is relatively sustainable, although the industrial processing requires attention to chemical management.
 |  |
Molecular Formula C12H22O11
Molecular Weight 342.30 g/mol
CAS 4618-18-2
UNII 9XH2P2N8EP
EC Number 225-027-7
DTXSID5045833
Synonyms:
D-Lactulose
References__________________________________________________________________________
(1) Lee-Robichaud H, Thomas K, Morgan J, Nelson RL. Lactulose versus Polyethylene Glycol for Chronic Constipation. Cochrane Database Syst Rev. 2010 Jul 7;(7):CD007570. doi: 10.1002/14651858.CD007570.pub2.
Abstract. Background: Constipation is a common clinical problem. Lactulose and Polyethylene Glycol (PEG) are both commonly used osmotic laxatives that have been shown to be effective and safe treatments for chronic constipation. However, there is no definitive data as to which provides the best treatment. .... Selection criteria: Studies were included if they were randomised controlled trials which compared lactulose with polyethylene glycol in the management of chronic constipation. Data collection and analysis: Data on study methods, participants, interventions used and outcomes measured was extracted from each study. Data was entered into the Cochrane Review Manager software (RevMan 5.0) and analysed using Cochrane MetaView. Main results: In the present meta-analysis, we considered for the first time all ten randomised controlled trials so far performed. The findings of our work indicate that Polyethylene glycol is better than lactulose in outcomes of stool frequency per week, form of stool, relief of abdominal pain and the need for additional products. On subgroup analysis, this is seen in both adults and children, except for relief of abdominal pain.
Steurbaut L, Levy EI, De Geyter C, Buyse S, Vandenplas Y. A narrative review on the diagnosis and management of constipation in infants. Expert Rev Gastroenterol Hepatol. 2023 Jul-Dec;17(8):769-783. doi: 10.1080/17474124.2023.2242255.
Abstract. Introduction: Functional constipation is one of the common disorders of gut-brain interaction in infancy, and decreases the quality of life of infants and parents. Areas covered: Relevant articles up to November 2022 were reviewed. We searched in PubMed, Google Scholar, and MEDLINE for guidelines, position papers, reviews, and randomized controlled trials on infant constipation. Expert opinion: Randomized controlled trials in this specific age group are mostly limited to trials with infant formula. The prevalence of infant constipation in formula-fed infants is decreasing, and can be associated with adaptations in formula composition. While the supplementation of infant formula with pro-, pre- and/or synbiotics decreases the prevalence of constipation, their efficacy in constipated infants is disappointing. There is limited evidence to support the addition of magnesium to infant formula to treat constipation. The evidence for the efficacy and safety of polyethylene glycol in children < 2 years has expanded over the past years. The administration of lactulose or polyethylene glycol is the preferred medical management, in case nutritional management does result in insufficient improvement.
Maydeo A. Lactitol or lactulose in the treatment of chronic constipation: result of a systematic. J Indian Med Assoc. 2010 Nov;108(11):789-92.
Abstract. Constipation is a common problem for adults and paediatric patients and can generate considerable suffering for patients due to both the unpleasant physical symptoms and psychological preoccupations that can arise. Since disaccharide sugar is widely prescribed osmotic laxative in India, we decided to do systematic review to compare the efficacy and safety of lactitol versus lactulose in the management of constipation. All randomised, non-randomised and open trials, with head to head comparison of lactitol versus lactulose were included. After intense literature search we included six clinical trials for comparison. The relevant studies that were included in meta-analysis included 349 adult patients with mean age group of 19 to 85 years and 81 children from age group of 8 months to 16 years. Duration of treatment was 3 days to 4 weeks. In terms of efficacy lactitol was found to be comparable to lactulose in terms of normal consistency of stool and number of bowel movement per week. Better acceptance by the patients was reported with lactitol as compared to lactulose (73.2% versus 26.8%). Lactitol was found to be significantly superior as compared to lactulose in terms of less number of adverse events (31.20 +/- 0.8000% versus 62.10 +/-1.100%, p = 0.0019). Better efficacy was adjudged by the physicians in favour of lactitol as compared to lactulose (61.91% versus 47.83%). In addition compliance with lactitol was found to be better due to superior palatability. Also in paediatric patients the dose of lactitol required was almost half the dose of lactulose (250-400 mg/kg/day versus 500-750 mg/kg/day). Lactitol should be preferred over lactulose in the management of chronic constipation because of its superior efficacy as adjudged by the physician, better palatability, lesser incidence of adverse events, better acceptance and compliance reported by patients.
(2) Hudson M, Schuchmann M. Long-term management of hepatic encephalopathy with lactulose and/or rifaximin: a review of the evidence. Eur J Gastroenterol Hepatol. 2019 Apr;31(4):434-450. doi: 10.1097/MEG.0000000000001311.
Abstract. A consolidated overview of evidence for the effectiveness and safety/tolerability of hepatic encephalopathy (HE) treatment over the long term is currently lacking. We identified and assessed published evidence for the long-term (≥6 months) pharmacological management of HE with lactulose and/or rifaximin. A literature search was conducted in PubMed (cutoff date 05 March 2018) using the search terms 'hepatic encephalopathy+rifaximin' and 'hepatic encephalopathy+lactulose'. All articles containing primary clinical data were manually assessed to identify studies in which long-term (≥6 months) effectiveness and/or safety/tolerability end points were reported for lactulose and/or rifaximin. Long-term effectiveness outcomes were reported in eight articles for treatment with lactulose alone and 19 articles for treatment with rifaximin, alone or in combination with lactulose. Long-term safety/tolerability outcomes were reported in six articles for treatment with lactulose alone and nine articles for treatment with rifaximin, alone or in combination with lactulose. These studies showed that lactulose is effective for the prevention of overt HE recurrence over the long term and that the addition of rifaximin to lactulose significantly reduces the risk of overt HE recurrence and HE-related hospitalization, compared with lactulose therapy alone, without compromising tolerability. Current evidence therefore supports recommendations for the use of lactulose therapy for the prevention of overt HE recurrence over the long term, and for the additional benefit of adding rifaximin to lactulose therapy. Addition of rifaximin to standard lactulose therapy may result in substantial reductions in healthcare resource utilization over the long term, by reducing overt HE recurrence and associated rehospitalization.
Zucker DM, Redulla R. Lactulose Management of Minimal Hepatic Encephalopathy: A Systematic Review. Gastroenterol Nurs. 2019 Jan/Feb;42(1):84-94. doi: 10.1097/SGA.0000000000000429.
Abstract. Minimal hepatic encephalopathy has been shown to increase risk of involvement in road traffic accidents and alter quality of life. This systematic review focused on the role of nonabsorbable disaccharides for the management of minimal hepatic encephalopathy. Randomized clinical trials that evaluated medical management of minimal hepatic encephalopathy were considered for inclusion. Individual studies compared lactulose with usual care and lactulose with probiotics and L-ornithine-L-aspartate. The outcome for examination was the neuropsychiatric test for cognitive function. Search strategies outlined by the Johanna Briggs Institute were used, and articles and references of selected articles were reviewed according to that methodology. Meta-analyses and narrative synthesis of the included studies were undertaken. Treatment of minimal hepatic encephalopathy with lactulose, probiotics, or L-ornithine-L-aspartate was seen to be equally effective in reducing abnormal tests at 1, 3, and 12 months post-treatment. All patients with minimal hepatic encephalopathy should be screened using a neuropsychiatric test and receive treatment as needed. Treatment can delay or eliminate risky automobile accidents and harm to self. Lactulose, probiotics, and L-ornithine-L-aspartate are a low-cost alternative compared with antibiotic treatment.
Wijdicks EFM. Lactulose: A Simple Sugar in a Complex Encephalopathy. Neurocrit Care. 2018 Apr;28(2):154-156. doi: 10.1007/s12028-017-0494-4.
Abstract. Hepatic encephalopathy is a common encephalopathy and one of the very few that are treatable. Lactulose has remained a standard pharmaceutical intervention and is listed as one of the World Health Organization's Essential Medicines. The discovery of lactulose, the acid dialysis proof of concept, and the role of Bircher are not well known. This historical vignette reviews the gradual understanding of the complex liver-brain connection, the effective treatment of hepatic stupor with lactulose, and the immediate relevance of lactulose to the practice of consultative neurocritical care.
| Evaluate |
