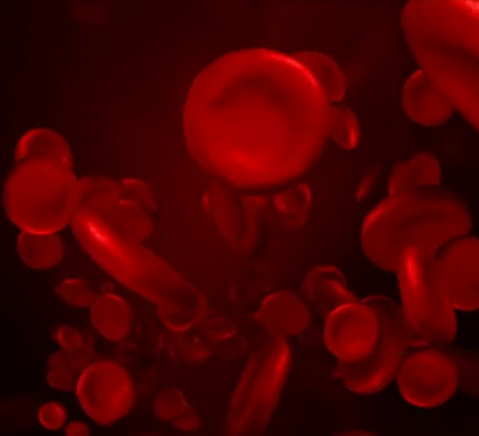
![]() Eritrociti
Eritrociti
Rating : 10
| Evaluation | N. Experts | Evaluation | N. Experts |
|---|---|---|---|
| 1 | 6 | ||
| 2 | 7 | ||
| 3 | 8 | ||
| 4 | 9 | ||
| 5 | 10 |
10 pts from Kevin-Wooderly
| Sign up to vote this object, vote his reviews and to contribute to Tiiips.Evaluate | Where is this found? |
| "Descrizione" about Eritrociti Review Consensus 10 by Kevin-Wooderly (155 pt) | 2021-Jan-29 19:48 |
| Read the full Tiiip | (Send your comment) |
English translation and modification in some non-substantial points of Ivan's review
Erythrocytes originate from a common progenitor in the bone marrow, the hematopoietic stem cell, through a process of erythropoietic differentiation. They are formed from immature cells called erythroblasts. Erythropoietin (EPO) synthesized mainly in the kidney and released under hypoxic conditions into the bloodstream is the main regulatory factor of erythropoiesis. More details you will get from the histology course. The most important function of erythrocytes is the transport of oxygen to tissues and the elimination of carbon diox ide and protons produced by cellular metabolism. For this purpose, erythrocytes have a specialized membrane structure that gives the cell a biconcave shape particularly suited to the plasticity and deformability required to pass through small caliber capillaries and the increased surface area/volume ratio important for gas exchange.
ide and protons produced by cellular metabolism. For this purpose, erythrocytes have a specialized membrane structure that gives the cell a biconcave shape particularly suited to the plasticity and deformability required to pass through small caliber capillaries and the increased surface area/volume ratio important for gas exchange.
The average life of normal erythrocytes is 120 days, which means that every day a number of red blood cells equal to 1% of the total population is replaced. The new erythrocytes that appear in the circulation have lost the nucleus but still contain ribosomes and elements of the endoplasmic reticulum, and are called RETIC OLOCITI, they are the immature erythrocytes, they still have an active protein biosynthesis. The RNA of the ribosomes can be stained with methylene blue. The number of reticulocytes is about 1% of total erythrocytes. In case of hemolytic anemias we will have increased circulating reticulocytes, because there is increased erythropoiesis to compensate for the increased destruction of red blood cells. The opposite situation occurs in anemias from lack of production, in which the number of reticulocytes will decrease. The assay of circulating reticulocytes allows the differential diagnosis between anemias in which there is increased loss or destruction of red blood cells from those in which there is decreased red blood cell production.
Mature erythrocytes are cells lacking a nucleus and other cellular organelles, such as lysosomes, ribosomes, Golgi apparatus, and mitochondria. Therefore, mitochondrial oxidative phosphorylation does not contribute to ATP formation, only glycolysis. Glucose is their only source of energy. They have a half-life of 120 gg and are eliminated by the spleen and bone marrow. They accumulate damage mainly to the membrane, and when senescent they assume a spherical shape that is recognized by splenic macrophages.
Some important parameters of red blood cells describe the size of the cells and the protein content of hemoglobin, which carries oxygen MCV (volume): measures the size (normal value: 82-98 fentoliters) MCHC (mean corpuscolar hemoglobin concentration): average concentration of hemoglobin in cells, correlated with cell color (normal value: 31-37 g/dl) RDW (red cell distribution width): measures variation in red cell size, i.e., anisocytosis (normal value: 11.5-14.5%).
Red blood cells have a biconcave disk shape, in order to allow the maximum gas exchange, in fact we

have the maximum surface/volume ratio; they are anucleated; they are made up of 95% of hemoglobin; and they travel during their life about 300 400 km. They are highly deformable cells: 13 are able to pass in capillaries with a diameter smaller than that of the red blood cell because they are able to crush and are highly elastic so as to return to their original form.
The change in size of red blood cells is called Anisocytosis. The increase in the number of abnormally shaped red blood cells is called Poikilocytosis. Normocytic is the red blood cell of normal size. Normocytic is the red blood cell with normal hemoglobin concentration.
Erythrocyte Metabolism
Red blood cells possess a peculiar and relatively simple metabolism. They depend on glucose as their primary energy source. ATP is produced in glycolysis, which proceeds to lactate. The synthesis of 2,3-biphosphoglycerate, which proceeds through reactions closely associated with glycolysis, is important in regulating the ability of hemoglobin to transport and release oxygen. In erythrocytes, the pentose phosphate pathway is active (approximately 5-10% of glucose is metabolized through this pathway) and serves to produce NADPH, which is required to return oxidized glutathione (G-S-S-G) to its reduced form (GSH).
Most important aspects of erythrocyte metabolism.
ENERGY METABOLISM (GLYCOLYSIS);
DEFENSE AGAINST OXIDANT RADICALS (PENTOSE CYCLE);
Hb regulation (2-3 DPG);
HCO3- PRODUCTION / CO2 TRANSPORT;
NITRIC OXIDE TRANSPORT.
The red blood cell requires an energy source to:
1) maintain Hb iron in a reduced form (Fe++);
2) maintain high levels of K+ and low levels of intracytoplasmic Ca++;
3) maintain reduced sulfhydryl groups of Hb, enzymes and membrane;
4) maintain biconcave shape.

The red blood cell membrane contains glucose transporters with high affinity. Lactate formed as a terminal product of anaerobic glycolysis effluxes from the red blood cell and is sent to the liver via the Cori cycle.
Oxidant Radical Defense
The defense against oxidative radicals is provided by the pentose cycle, which produces in the oxidative phase the NADPH necessary for glutathione reduction. The pathway of pentose-phosphates is the only way to produce NADPH for the red blood cell, the red blood cell is very sensitive to oxidative damage when the functionality of this metabolic pathway is compromised for example, by an enzymatic deficiency of glucose-6-phosphate dehydrogenase. The red blood cell produces several oxygen radicals with high oxidative power. First, it produces the superoxide anion, which is formed by auto-oxidation of hemoglobin to methemoglobin. The heme of hemoglobin possesses reduced iron (Fe2+). A very small proportion of the iron (1-2%) is oxidized to Fe3+, the oxygen receiving an electron from the reduced iron is transformed into superoxide anion. Hemoglobin becomes methemoglobin, which is no longer able to transport oxygen. The superoxide anion can produce other free radicals. Superoxide anion dismutation is the reaction that occurs between two superoxide anion molecules: one of these molecules, giving up the electron, becomes O2; the other, accepting the electron, is reduced in a bivalent fashion, forming hydrogen peroxide H2O2 (hydrogen peroxide). Hydrogen peroxide then can give rise to the more dangerous OH hydroxyl radicals. The chemical species hydroxyl radical and OH- can be formed from hydrogen peroxide molecules in an enzymatic reaction catalyzed by Fe2+: the Fenton reaction. In the Fenton reaction, the electron donor to hydrogen peroxide is bivalent free iron. High concentrations of free iron or diseases such as hemochromatosis (accumulation of iron in tissues due to a genetic defect) can cause free radical damage. Superoxide anion and hydrogen peroxide are the substrates of the Haber-Weiss reaction that produces hydroxyl radical and OH-. The superoxide anion gives up the electron to the hydrogen peroxide molecule, which, upon receiving the electron, splits into two molecules: the hydroxyl ion (OH-) and the hydroxyl radical.
Free radical defense systems
The erythrocyte is therefore damaged both because of the formation of superoxide anion and because it can no longer transport oxygen. The enzyme methemoglobin reductase is capable of reducing iron to its bivalent form and regenerating hemoglobin, thus limiting free radical damage. The enzyme superoxide dismutase accelerates the dismutation reaction of the superoxide anion, which converts to hydrogen peroxide or hydrogen peroxide. Glutathione, with its sulfhydryl group, serves to reduce hydrogen peroxide, thanks to glutathione peroxidase becomes oxidized glutathione (GSSG), two GSH molecules joined by a disulfide bridge. This is then reduced to two molecules of GSH thanks to glutathione reductase, which uses NADPH produced in the phosphate pentose pathway. Hence the importance of NADPH in maintaining reduced glutathione levels and preventing oxidative damage. A reduction in Glucose-6-phosphate dehydrogenase can result in hemolytic anemia.

Microscopic visualization of sickle cells causing anemia disease
Glutathione peroxidase, a selenium-containing enzyme, catalyzes the reaction of both hydrogen peroxide and lipid peroxides. It is present in all tissues, but is particularly abundant in the red blood cell. There is also another enzyme, catalase, which can turn two molecules of hydrogen peroxide into 2 molecules of water and oxygen.
Meta-Hemoglobinemia or Methemoglobinemia
In Methemoglobinemia, heme iron is found in the form of ferric ion rather than ferrous ion. Methemoglobin, or methemoglobin, is a form of metal-protein hemoglobin, in which the iron in the heme group is in the Fe3+ (ferric, hemichromes) state, not Fe2+ (ferrous, heme) of normal hemoglobin. The change in oxidation state deprives the molecule of its ability to bind oxygen, and thus it also loses its physiological function of transporting oxygen. In human blood a trace amount of methemoglobin is normally produced spontaneously, but when present in excess the blood becomes abnormally dark bluish brown, cyanotic. The NADH-dependent enzyme methemoglobin reductase is responsible for the conversion of methemoglobin to hemoglobin. Methemoglobin reductase is a cytochrome b5-containing flavoprotein. Methemoglobinemias can be acquired (oxidizing agents, parasitic infections such as malaria plasmodium), inherited (hemoglobin M), or a consequence of reduced methemoglobin reductase activity. The heme of methemoglobin is called a hemichrome; the distal histidine E7 binds covalently with the ferric ion. Hemichromes are dangerous and damaging to the membrane; hemichromes detach from the hemoglobin globin, which has a deeply altered, denatured tertiary structure, and attach to band 3 and are potent generators of oxygen radicals.
Plasmodium malaria infection
In the course of infection with malaria plasmodium, many aggregates of hemichromes with band 3 are formed, which are recognized by natural antibodies (autoantibodies), which eliminate erythrocytes. These aggregates also form in aged red blood cells. These hemichromes lead to destabilization of the erythrocyte membrane with increased vesiculation, membrane leakage, and microcytosis. These mechanisms are of low intensity in uninfected GR, but are greatly enhanced in GR with mutated hemoglobins, such as hemoglobin C. One explanation for the mechanism of malaria resistance, which is similar in both hemoglobinopathies and G6PD deficiency, is the strong increase in methemoglobin and macromolecular aggregates (hemichromes) that ultimately induce band 3 aggregation, deposition of anti-band 3 autoantibodies and complement factors (C3c), ring opsonization and phagocytic removal of early forms of the parasite from resident and circulating phagocytes. G6PD enzyme deficiency causes nonspherocytic hemolytic anemia.

Red Blood Cell Deficit
G6PD
The gene that codes for G6PD is the target of several mutations. Many mutations result in the enzyme working less and being degraded faster than normal. Red blood cells, being anucleated, lack the ability to synthesize enzymes, and over time their enzyme pool decreases. If an individual has a mutated G6PD such that the enzyme works less and lives less, the red blood cells will be more prone to oxidative damage from ROS. This is not a problem in nucleated cells, but in the red blood cell it is. This is why a G6PD-deficient person if they don't take particular medications or foods (like fava beans) will have no problems. However, if this happens, ROS can overcome the accumulated reserves of glutathione and NADPH and go to hit the cell membranes of red blood cells → hemolysis. The G6PD mutation is an X-linked disease, hemizygous males and homozygous females, with variable expression in heterozygous females due to random inactivation of the X chromosome. The mutation confers protection against malaria. More than 300 genetic variants are known, with more than 400 million people worldwide having this deficiency. Total enzyme deficiency gives hemolytic anemia, but usually G6PD also works around 2% of its maximum possibilities and therefore we can have several less severe forms. This deficiency is widespread because, if you do not take fava beans or particular medications you do not have problems therefore, the individual can survive and pass on the gene. In addition, G6PD deficient subjects survive better than healthy subjects where malaria is endemic. This is because it has been seen that G6PD deficient subjects create a less favorable environment for the malaria parasite to establish itself. It is a case of what in genetics is called balanced polymorphism.
The diagnosis of G6PD deficiency is typically suspected when a patient of a certain ethnicity exhibits jaundice and signs of hemolysis following one of the triggers. G6PD deficiency is also called 3 A's disease as it can be caused by Antimalarials, Antibiotics, or Aspirin. In fact, affected individuals may experience non-immune hemolytic anemia in response to numerous causes, most commonly infections or exposure to certain chemicals or drugs. G6PD deficiency is closely related to favism, a clinical manifestation characterized by a hemolytic crisis in response to fava bean consumption. Treatment consists of transfusions and hydration (hemoglobin can precipitate and cause kidney problems).

G6PD deficits due to mutations are very frequent in certain regions of the world: tropical Africa, the Mediterranean, certain parts of Asia. G6PD-deficient erythrocytes parasitized by the plasmodium are more rapidly eliminated by the reticuloendothelial system present at the splenic level. Therefore, the mutation constitutes in the areas of origin of these individuals, where malaria is endemic, a significant evolutionary advantage by giving individuals carriers a better biological fitness. The hemoglobin forms aggregates visible under the microscope (Heinz bodies). The sulfhydryl groups of hemoglobin are oxidized giving rise to the formation of cross-links that increase the formation of insoluble aggregates already seen called hemichromes, which condense on the band 3 with the consequent elimination of red blood cells (hemolysis).
Hemolytic anemia due to pyruvate kinase (PK) deficiency
Hemolytic anemia from pyruvate kinase deficiency in erythrocytes is a rare (1/100000) metabolic disease. PK is a key enzyme in glycolysis. Deficiency results in ATP depletion and increased concentration of 2,3 DPG. 31. Patients suffer from chronic hemolysis of varying degrees; jaundice, stones, and splenomegaly are also common here.
The transport performed by erythrocytes
The red blood cell transports protons and bicarbonate. In addition to carrying oxygen, hemoglobin also transports two end products of cellular respiration, H+ and CO2, from the tissues to the lungs and kidneys.
Carbon dioxide is a neutral molecule, which can cross the erythrocyte membrane and penetrate into the interior of the cell. Transport is facilitated by membrane transporters. CO2 produced during cellular respiration is converted to carbonic acid, which dissociates to bicarbonate ion and H+. Carbonate synthesis is catalyzed by carbonic anhydrase, an enzyme particularly abundant in erythrocytes. The formation of protons resulting from the reaction catalyzed by carbonic anhydrase leads to a lowering of the pH. In turn, pH affects the affinity of oxygen for hemoglobin, and bicarbonate formation becomes an important process in regulating oxygen transport in the blood. Like 2,3 DPG, the H+ ion and CO2 are allosteric effectors that bind to hemoglobin at sites distinct from oxygen binding sites. The regulation of oxygen binding by H+ ions and carbon dioxide goes by the name of the Bohr effect, which we will see in a moment. Most of the carbon dioxide is transported in the form of HCO3-, which is formed by hydration of carbon dioxide within the red blood cell. The bicarbonate thus formed is transported outside the cell by a specific transporter, located on the erythrocyte membrane (called band 3), which exchanges the intracellular HCO3- with the extracellular Cl- ion.
In the lungs, the process is reversed: bicarbonate is transported back into the erythrocyte with the release of Cl-, it is reconverted, via carbonic anhydrase, into carbon dioxide, which is then eliminated through respiration. The binding of oxygen to haemoglobin in the lungs promotes the elimination of CO2 (the Haldane effect, which you have already seen, depends on CO2 being eliminated as a gas). More specifically, as the pH decreases, the affinity of oxygen for haemoglobin decreases. Thus, the transport of oxygen from the lungs, where the partial pressure of oxygen is 100 Torr and the pH is 7.4, to the contracting muscle, where the partial pressure of oxygen is 20 Torr and the pH is 7.2, results in the release of a quantity of oxygen equal to 77% of the total transport capacity. If there were no pH variation between the lungs and the working muscle, the release capacity would only be 66%.

Transportation NO
L’emoglobina rilascia ossido di Azoto (NO) alle pareti dei capillari dei tessuti a cui rilascia ossigeno. L’emoglobina lega reversibilmente l’ossido di azoto, un potente vasodilatatore con una brevissima emivita nel sangue. Questo legame lo preserva da una rapida distruzione. L’emoglobina rilascia l’NO nel passaggio dalla conformazione R alla T (fase 6 e 7 della slide), e lo trasferisce a piccole molecole con gruppi SH come il glutatione. L’NO, sotto forma di X-S-NO risulta stabilizzato e può essere efficacemente essere rilasciato come molecola bioattiva ai recettori dell’NO delle cellule delle pareti dei vasi, dove promuove il rilasciamento della parete vascolare. Tale rilasciamento facilita il trasferimento di gas fra il sangue e le cellule dei tessuti. A causa delle concentrazioni molto base di NO nel sangue, solo una molecola di emoglobina su 1000 è coinvolta in questo trasporto.
Haemoglobin
The cooperativity of the oxygenation curve means that binding to one of the four haemoglobin sites affects the binding properties of the other three. Haemoglobin exists in two conformational states: the R (relaxed) state and the T (tense) state. Oxygen can bind to haemoglobin in both states, but the affinity of the R state for the ligand is much higher. Oxygen binding to the protein stabilises the R state. When oxygen is not available, the T state is more stable, and so this is the predominant conformation of deoxyhaemoglobin. The T state is stabilised by a greater number of salt bridges, many of which are located at the α1β1 and α2β2 interface. 38. Haemoglobin in the T state is so unstable that in the presence of oxygen the whole protein would be in the R state. As a consequence, the equilibrium would be shifted to the R state and thus haemoglobin would not be able to release oxygen to tissues.
DPG or BPG (diphosphoglycerate/biphosphoglycerate)
In order to stabilise the T-state within red blood cells there is a substance called 2,3 bisphosphoglycerate or 2,3 BPG (or DPG). 2,3 BPG plays an important role in physiological adaptation to low O2 pressures, such as occur at high altitudes. If a person is transported rapidly up a mountain where oxygen pressure is considerably lower than at sea level, oxygen transfer to the tissues is reduced. A few hours later, the concentration of 2,3 BPG begins to increase, leading to a decrease in haemoglobin's affinity for oxygen. 39.BPG is linked to gluconeogenesis and glycolysis: 2,3-BPG is formed from 1,3-BPG (glycolytic intermediate) by the enzyme called bisphosphoglycerate mutase. In humans, 2,3- bisphosphoglycerate phosphatase catalyses the conversion 2,3-BPG + H2O → 3-phosphoglycerate + PO4 followed by a shift of the phosphoric group to position 2 by a mutase (Phosphoglycerate mutase): 3-phosphoglycerate → 2-phosphoglycerate.
This strongly anionic compound has a concentration of 5 mM in red blood cells, approximately equal to that of haemoglobin to which it binds in a 1:1 ratio in a pocket of the haemoglobin tetramer in the T conformational state. This pocket is lined with amino acids with positively charged R groups that interact with the negatively charged groups of 2,3 BPG. As a result of the transition from the T to the R state, the pocket contracts and 2,3 BPG is released: this is the consequence of the breaking of bonds between 2,3 BPG and haemoglobin. By stabilising the T state, 2,3 BPG lowers the affinity of oxygen for haemoglobin and is therefore a negative allosteric effector. When haemoglobin reaches the tissues, the β-chains are the first to release oxygen and this loss leads to a displacement of monomers from the centre. As soon as the hydrophilic cavity opens, BPG enters and binds to the tetramer. In the lungs, the reverse process occurs. At high oxygen pressure, the BPG is 'squeezed' and expelled from the tetramer, allowing easier oxygen-β-chain binding. The regulation of oxygen affinity for haemoglobin by 2,3 BPG has an essential function in fetal development. Since the fetus 'extracts' oxygen from maternal blood, fetal haemoglobin must have a higher affinity for O2 than maternal haemoglobin. In fact, in the fetus, instead of β-subunits, γ-subunits are produced and a haemoglobin with an α2γ2-subunit composition is formed. This tetramer, called fetal haemoglobin, has a very low affinity for 2,3 BPG and consequently a higher affinity for oxygen. The intraerythrocyte pH is the main regulator of BPG level. The intraerythrocyte pH rises during hypoxia (alkalosis). Hypoxia causes hyperventilation and increased CO2 elimination. The concentration of BPG in erythrocytes also increases in cardiopulmonary insuffiency and anaemia.

Erythrocytes membrane
The cytoplasmic membrane of erythrocytes is well known. The erythrocyte must be able to deform to pass through very small capillaries. Bound to the inner side of the erythrocyte membrane are some peripheral cytoskeleton proteins, the spectrins, which form a hexagonal meshwork where another protein, ankyrin, binds the spectrin to the membrane. The membrane is a lipid bilayer consisting of 50% lipids and 50% proteins. Ankyrin-1 binds the spectrin β-chain, protein 4.2 and band 3, thus ensuring the attachment of the spectrin to the membrane. Glycophorin A is an erythrocyte-specific marker. The Rh complex (B) consists of the Rh protein (Rh), the Rh-associated glycoprotein (RhAG), CD47 and the Landsteiner-Wiener glycoprotein (LW). CD47 interacts with protein 4.2 and Rh protein to contact ankyrin-1. The junctional complex (C) consists of band 4.1, spectrin, actin, dematin (4.9), tropomyosin and β-adducin (not shown). Spectrin (D) is the main protein of the cytoskeleton, it is an α2β2 tetramer that forms a dense network lining the inner surface of the lipid bilayer. The α and β chains are anti-parallel; the dimers associate side-by-side and head-to-head. N-terminal of α-chains and C-terminal of β-chains. Peripheral cytoskeleton proteins play an important role in maintaining the shape and flexibility of the cytoskeleton.
There are some haemolytic anaemias due to membrane defects, in which the cytoskeleton-membrane complex is altered. An example is hereditary spherocytosis. SDS-PAGE analysis allows the membrane proteins of erythrocytes to be resolved, about ten major protein bands are resolved. These proteins were named according to their speed of migration in SDS-PAGE: the slowest migrating band, corresponding to the protein with the highest molecular weight, was referred to as Band 1 or spectrin. All these proteins were isolated and identified for their biological role. Several types of diseases associated with membrane disorders, such as spherocytosis or ellipsocytosis, have been identified.
Erythrocyte diseases
Hereditary spherocytosis
Hereditary spherocytosis is a relatively common haemolytic anaemia in northern Europeans and North Americans (1:5000) that is inherited as an autosomal dominant and recessive trait. The red blood cell has a spherical, non-functional shape.
Genetic defects affect:
1) band complex 3 - actin - spectrin;
2) complex 4.1 - spectrin - glycophorin;
3) the connection between the bilayer and the spectrin.
A reduced surface to volume ratio occurs. Spherocytes are less flexible, have a high susceptibility to lysis and are destroyed in the spleen (splenomegaly). Vesicles are formed and lost from the surface of the red blood cell, resulting in a decreased surface area and a change in shape (spherocytes). There are also several mutations in the gene for the chloride/bicarbonate anion exchanger known as Band 3 or Solute Carrier Family 4 Member 1 (SLC4A1), which can give the typical hereditary spherocytosis (HS) or other forms of anaemia (SAO Southeast Asian Ovalocytosis; CHC: Cryohydrocytosis). This exchanger is also present in the basolateral membrane of the alpha intercalated cells of the distal renal tubule, and a mutation -DRTA- gives distal renal tubular acidosis.
Hereditary spherocytosis can occur in varying degrees of severity. Severe cases can occur as early as childhood with severe anaemia, whereas milder cases can appear in young adults or even later in life. Splenic sequestration of spherocytes (the more severe the deficiency of erythrocyte membrane proteins) and their subsequent phagocytosis by splenic macrophages cause the characteristic triad of ES: anaemia with reliculocytosis, jaundice and splenomegaly. In milder cases the anaemia is often compensated, but can easily decompensate (e.g. infection). It is usually a normocytic and normochromic anaemia. A typical finding is increased mean corpuscular haemoglobin concentration (MCHC). If the family history is positive, diagnostic suspicion is usually easy, but for at least two reasons there may be no family history:
1. the patient may have an ex novo mutation;
2. the patient may have a recessive form of spherocytosis.
In most cases, the diagnosis is confirmed on the basis of erythrocyte morphology and the osmotic fragility test. This test measures the extent of haemolysis that occurs when the red blood cell sample is subjected to osmotic stress in a hypotonic solution (decreasing concentrations of NaCl). Erythrocytes swell sooner with water than normal ones. The severity of symptoms is measured by haemoglobin levels, the number of reticulocytes and bilirubin levels. Possible complications of the disease may be: Parvovirus B19 aplastic crisis and Biliary calculosis.
Ellipsocytosis
In hereditary ellipsocytosis the red blood cells have an elliptical shape. It is due to spectrin or band 4.1 deficiency.
Hereditary stomatocytosis
Hereditary stomatocytosis is a rare anaemia with mouth-shaped red blood cells. It is due to an altered permeability of the membrane to sodium (Na+) and potassium (K+) ions.
Sickle Cell Anemia
Sickle cell anaemia is the most important haemoglobinopathy. We have already discussed it in the first half. The glutamate in position 6 of the beta chain is replaced by a valine. Subjects homozygous for HbS show sickle cell anaemia, in which haemoglobin molecules precipitate to form polymers that aggregate into tubular fibres and deform the erythrocyte, which takes on the characteristic sickle shape and occludes the vessels. It is the deoxygenated form of Hb S that has extremely low solubility. The valine side chain interacts with a complementary hydrophobic pocket on the β1 chain of another haemoglobin molecule. This complementary site is exposed in deoxygenated haemoglobin but not in oxygenated haemoglobin. This pocket is too small to contain glutamate, but valine is inserted. Deoxy-haemoglobin polymers are then formed, which precipitate.
Thalassaemias
Thalassaemias are genetic defects in haemoglobin synthesis. There is a decreased synthesis of one of the two globins (alpha or beta). The imbalance in globin chain synthesis leads to depression of haemoglobin production and precipitation of excess (toxic) globin. "Ineffective erythropoiesis". Various degrees of severity from asymptomatic to incompatible with life (hydrops fetalis). Found in people of African, Asian and Mediterranean descent. On smear, red blood cells are microcytic/hypochromic, deformed, abnormal haemoglobin electrophoresis (increase HbA2, HbF). Severe syndromes may have inclusions of Heinz bodies in the red blood cells. Fe deposits are generally high. The only treatments are stem cell transplantation and simple transfusion. Chelation therapy to avoid iron overload must be started early.
| Sign up to vote this object, vote his reviews and to contribute to Tiiips.EvaluateClose | (0 comments) |
Read other Tiiips about this object in __Italiano (1)
Last update: 2021-01-22 09:49:35 |